Over the past several decades, the health of the average American has steadily declined, marked by rising rates of obesity, diabetes, and other chronic conditions. Since the 1960s, obesity rates have tripled, with over 40% of U.S. adults classified as obese, and diabetes has surged from less than 3% of the adult population in 1980 to more than 11% today.
These are not merely individual challenges but national ones, placing immense strain on the U.S. healthcare system. Chronic diseases—many of which are tied to poor diet—account for 90% of the nation’s $4.5 trillion in annual healthcare spending. According to the Centers for Disease Control and Prevention (CDC), obesity alone costs the U.S. healthcare system nearly $173 billion a year, while diabetes, heart disease, and stroke costs an estimated $835 billion in medical costs and lost productivity.
The consequences of these health crises are glaring when compared to other wealthy nations. Despite spending more on healthcare per capita than any other country, the U.S. lags behind its peers in life expectancy. According to the Organisation for Economic Co-operation and Development (OECD), the U.S. spends $12,555 per capita annually on healthcare—56% more than the next highest-spending country—but ranks just 34th in life expectancy.
Amidst these alarming statistics, a cultural shift is gaining momentum: the call to “Make America Healthy Again.” Central to this movement is a focus on improving dietary habits, as research increasingly highlights the profound impact of diet on overall health. From reducing sugar, processed foods, and alcohol intake to incorporating more fruits, vegetables, and healthy proteins, Americans are beginning to embrace changes that could reverse decades of poor health outcomes. However, diet and the associated health outcomes vary significantly by region, reflecting broader cultural, economic, and demographic differences across the country.
The Prevalence of Diet-Related Health Conditions by State
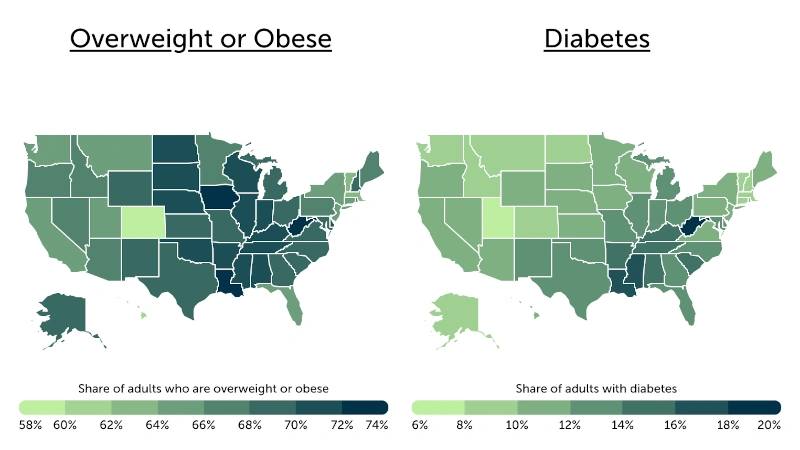
Analysis of CDC data. Credit: Trace One
Obesity is a major public health challenge across the U.S., but its impact is most pronounced in Southern and Midwestern states. States like West Virginia (73.2%), Iowa (72.1%), and Louisiana (72.0%) report the highest prevalence of overweight or obese adults. These figures are substantially higher than those observed in states like Colorado (59.8%) and Hawaii (60.5%), which have the lowest rates in the nation.
Similarly, diabetes prevalence, 90–95% of which is type 2 diabetes—a form largely preventable or manageable through lifestyle changes such as healthier diets and increased physical activity—is significantly higher in the South than in other regions. States like West Virginia (18.2%), Mississippi (17.0%), and Louisiana (16.1%) report the nation’s highest overall diabetes rates. In stark contrast, certain Western states such as Utah (7.8%), Colorado (8.6%), and Alaska (8.7%) have prevalence rates that are about half of those observed in the South.
Similar trends are evident for other diet-related chronic conditions, including high cholesterol, hypertension, and cardiovascular disease, where Southern and Midwestern states consistently exceed national averages in prevalence rates. In West Virginia, for instance, the proportion of adults who have experienced either coronary heart disease or a heart attack is approximately 75% higher than the national average.
Food Insecurity and Its Impact on Diet
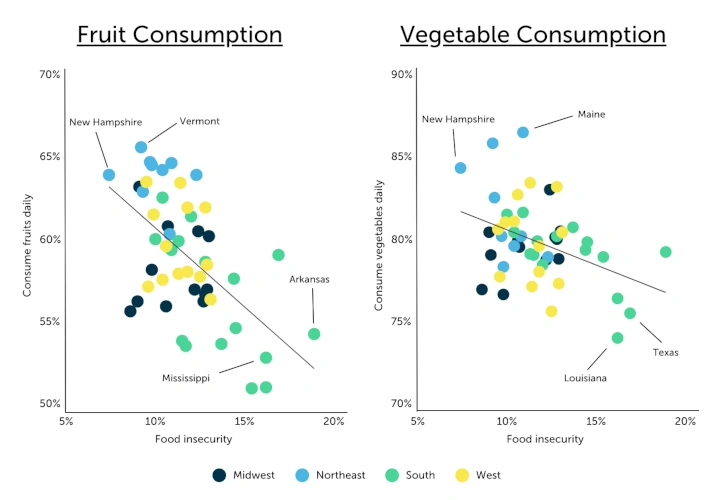
Analysis of CDC data. Credit: Trace One
The same regional patterns that define disparities in chronic health conditions also manifest in food access and dietary habits. Southern and Midwestern states, where obesity, diabetes, and cardiovascular disease rates are highest, consistently report lower consumption of fruits and vegetables and higher reliance on sugar-sweetened beverages and other processed foods. These dietary habits are influenced by socioeconomic factors, including food insecurity, which is disproportionately prevalent in these regions and significantly impacts the availability and affordability of nutritious options.
Food insecurity—defined as lacking consistent access to sufficient food—affects 12.2% of U.S. households, according to the U.S. Department of Agriculture (USDA). However, in states like Arkansas (18.9%), Texas (16.9%), Mississippi (16.2%), and Louisiana (16.2%), food insecurity rates far exceed the national average. In these areas, families often turn to cheaper, calorie-dense foods, exacerbating poor dietary habits and limiting the intake of nutrient-rich fruits and vegetables. This dynamic fuels a cycle of poor nutrition, contributing to the region’s elevated rates of diet-related chronic diseases.
In contrast, states with lower levels of food insecurity often report healthier eating patterns. New England states such as Vermont, Maine, and New Hampshire consistently lead in fruit and vegetable consumption, with over 64% of adults consuming fruits daily and over 84% eating vegetables daily. These states also report food insecurity rates well below the national average, reflecting how improved access to affordable, nutritious food supports healthier dietary choices.
Editor’s Note: The health challenges facing the United States are deeply intertwined with dietary habits, regional disparities, and access to nutritious food. While some states are making strides toward healthier eating patterns and improved food security, others continue to grapple with high rates of obesity, diabetes, and other diet-related chronic conditions. Addressing these issues requires a multifaceted approach, focusing on improving access to healthy food, reducing food insecurity, and promoting lifestyle changes across the nation. As more Americans embrace the importance of a balanced diet and healthier habits, the hope is that these shifts will reverse the troubling health trends of recent decades and lead to a healthier future for all.
Methodology
The data used in this study comes from the U.S. Centers for Disease Control and Prevention’s Behavioral Risk Factor Surveillance System (BRFSS) and National Health Interview Survey, as well as the U.S. Department of Agriculture’s Economic Research Service.
Due to limitations with the CDC data, not all states report data on each factor every year. Because of this, the latest available data was used for each state. In the event of a tie, the state with the higher percentage of adults who consume fruits daily was ranked higher.
This data for this post is derived from U.S. States With the Healthiest Diets, which originally appeared in the PLM Compliance Blog.
Written by Federico Fontanella, PMP
Federico is a Product Manager with background in Software Engineering and more than 15 years of experience in software development, project management, and product management. In his role as Sr. Director of Product Management at Trace One, Federico applies his strong software engineering background coupled with excellent understanding of business and market needs to define new product categories, improve business processes, and innovate solutions. Specialties: Product Management, Project Management, Software Development, Strategy


